 The information which follows is the opinion of the named author(s).
The information which follows is the opinion of the named author(s).
It does not necessarily constitute the opinion of The Prostate Cancer InfoLink or of
CoMed Communications, Inc.
Three-Dimensional Conformal Radiation Therapy (3DCRT) for Prostate Cancer
Part 2 of 2
[divided only to help load time - go to Part 1]
Jeff M. Michalski, MD,
Carlos A. Perez, MD, and James A. Purdy, PhD
Radiation Oncology Center, Mallinckrodt Institute of Radiology,
Washington University Medical Center, St. Louis, Missouri
Originally Received July 6, 1996; Last Revised July 8, 1996
Introduction |
What is 3DCRT? |
How is 3DCRT planned? |
How is 3DRCT delivered? |
What are the side effects of radiation therapy? |
Is 3DCRT better than conventional radiation therapy? |
What studies are currently ongoing investigating 3DCRT for prostate cancer? |
What will the future hold for 3DCRT and the treatment of prostate cancer? |
References |
Editorial comment
Step 4: Virtual simulation in 3D treatment planning
Virtual simulation is a process in which the physician
uses the digital CT data to define normal
tissue and target volume contours to reconstruct the patient
in three dimensions on a video display terminal. The
physician and medical dosimetrist can interactively
manipulate the view of the patient and his anatomy to find an
optimal arrangement of radiation beams that will minimize
radiation of adjacent normal tissues. Computer software
tools, such as beam's-eye-view (BEV) and room view (RV)
displays, help in selecting the best radiation beam geometry.
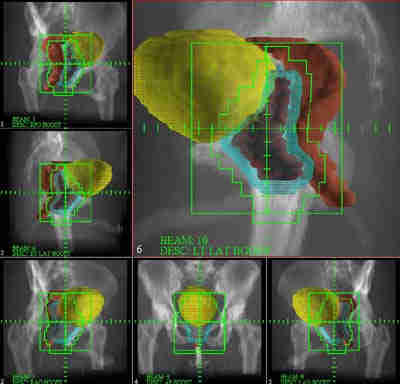
Figure 7. A beam's-eye-view (BEV) display allows the physician
to appreciate the tumor containing target from the same
perspective as the radiation treatment source. This
view allows the radiation oncologist to shape the
radiation field to the contour of the target's
silhouette. In this example, the stair step edges of
the field are a computer simulation of a multi-leaf
collimator (MLC). This stair step has little effect
inside the patient. The radiation scatter and
additive effects of multiple radiation beams smoothes
the radiation dose around the prostate tumor.
As implied, the BEV allows the clinician to look down the
radiation beam and see the target from the same perspective
as the radiation energy source. The RV display is helpful to
see the position of multiple beams and how they are oriented
relative to the patient. After the optimal beam projections
are chosen, the physician shapes the beam to the contour of
the target with the BEV display and a radiation dose is
assigned to each beam. The computer then sums the radiation
dose delivered from each projection and the physician and
dosimetrist can view the dose distribution with the RV tools.

Figure 8. A room-view display allows the radiation oncologist
to evaluate the relationship of multiple radiation
beams relative to the patient's anatomy and the target
volume. In this case six beams criss-cross and intersect within the prostate (red), behind the bladder (yellow), and in front of the rectum (brown).
 (a)
(a)
 9(b)
9(b)
Figure 9 The room-view display allows the physician to
evaluate the adequacy of radiation dose coverage of the
target volume. In Figure 9(a) the seminal vesicles were
not treated to the prescribed dose of 5580 cGy as
illustrated by the "birdcage" display. This
distribution was based on a two-dimensional treatment plan. Despite
this inadequate tumor coverage the rectum and bladder
are receiving a large dose. Figure 9(b) demonstrates the
effects of a conformal treatment plan. The prostate
and seminal vesicles received 5580 cGy but large
portions of the rectum and bladder are spared. The
treatment plan for this patient included an additional
"boost" to the prostate for a total dose of 7380 cGy
(not shown).
Another software feature that is helpful for 3DCRT,
although not mandatory, is the
digital reconstructive radiograph (DRR). This DRR tool
computes a "virtual radiograph" from the planning CT data.
The DRR looks like a plain X-ray but has the advantage of
displaying the target volumes and normal tissues contoured
from the CT scan data. This is very important for treatment
verification and quality assurance. The DRR can have the
radiation portal shape superimposed upon it. The DRR is used
to verify that treatment delivery is being done as planned.

Figure 10. The digitally reconstructed radiograph (DRR) is
computed from the CT data. This has a similar
appearance to a plain X-ray but allows concurrent
display of a patient's internal anatomy and radiation
target. The physician can use this DRR to verify the
adequacy of treatment delivery.
Another helpful tool in the evaluation of 3D radiation
therapy plans is the dose volume histogram (DVH). DVHs are
graphical display tools that allow a physician to quickly
estimate the dose of radiation delivered to normal tissues
and target volumes. They are extremely valuable when
comparing different radiation therapy techniques.

Figure 11. A dose-volume histogram allows the physician to
compare the quality of various treatment plans. These
tools allow a radiation oncologist to select a
treatment plan that maximizes radiation coverage of the
tumor while minimizing radiation dose to the normal
tissues. In this display the red curve demonstrates a
completely 3D conformal plan, the green curve a
"partially" 3D conformal plan, and the blue curve a
traditional, two-dimensional plan. For the normal tissues the
vertical bar represents a conservative estimate of the
expected organ tolerance. Those estimates were based
on historical experiences with inexact data from
traditional, two-dimensional therapies. The vertical bar on the target
volume curve represents the intended radiation dose
prescription. Each plan adequately covers the target
volumes but the most conformal plan (red) delivers
substantially lower doses of radiation to the normal
tissue volumes.
How is 3D conformal radiation treatment delivered?
As in conventional radiation therapy, 3DCRT
delivery is fractionated. A
course of radiation therapy is generally given over several
weeks in small daily fractions. Radiation fractions are
typically administered for 5 days/week for as many as 6.5-8 weeks
for curative prostate cancer therapy. A small
daily fraction, 1.8-2.0 Gy/d (1 Gy = 100 rad), allows
the normal tissues to recover between treatments whereas
tumor cells are less efficient at repairing radiation damage.
There are several acceptable methods for delivery of the
radiation treatments. Some institutions use four conformally
shaped fields directed at the prostate; two from the sides
and two angled from the front of the patients' feet. Others
use six to eight fields all directed from a single plane rotating
about the pelvis. Methods used by each institution are
selected based upon linear accelerator machine
characteristics. It is not clear that any one method is
physically superior to another. At the Mallinckrodt
Institute of Radiology we have been using a six- or seven-field
coplanar method for several years with good reliability and
clinical results. As the number of fields used to treat the
prostate increases, it is convenient to use automatic field
shaping devices in the head of the treatment linear
accelerator. A multi-leaf collimator (MLC) allows automatic
reshaping of the treatment field from outside the room while
the patient is being treated. The ease and speed of
automatic field shaping makes the delivery of complex
multiple field arrangements more efficient. It also
eliminates the hazards of handling heavy lead alloy blocks by
the radiation therapist.

Figure 12. A multi-leaf collimator (MLC) assists in the
shaping of the radiation beam. In this photograph the
MLC is removed from the head of the treatment delivery
machine (a linear accelerator). Data from the 3D
treatment plan is used to shape the radiation fields
with the MLC. This device allows the physician to use
multiple radiation beams to treat a patient in less
time than it generally takes to treat him with lead
alloy blocks. This added efficiency allows the
radiation oncologist to use more treatment fields to
shape the radiation dose inside the patient. In the
future this device will be used to modulate the
intensity of radiation beams and create even more
conformal treatment plans with increased protection of
the normal tissues and more intensive treatment of the
tumor.
What are the side effects of radiation therapy?
Generally, few if any side effects accompany the first
few weeks of radiation therapy. X-rays are not felt or seen
as the linear accelerator moves about the patient delivering
X-rays. Gradually, after 2-3 weeks of therapy, side
effects may begin to develop. They are generally confined to
the treatment area. Bladder and rectal irritation can occur,
giving the patient an urge to urinate more frequently,
especially at night, or to have more frequent bowel
movements. Sometimes a burning or stinging sensation
accompanies bowel movements or bladder emptying. There can
be loose stools or diarrhea.
In general, most of the side effects
associated with radiation therapy are mild, especially when
administered with 3DCRT techniques.
If they do occur they can often be managed with medications or
dietary modifications. Some men may have diarrhea
precipitated by high fiber foods, dairy products, or high fat
foods. Changing to a low residue, lactose-free, or low-fat
diet may help identify the aggravating dietary factor.
In most men the acute side effects resolve within 4-6
weeks after radiation therapy is completed. Some men may
need to use hemorrhoidal preparations or sitz baths to
alleviate anal/rectal discomfort for longer than that.
Occasionally, food intolerances are identified during
treatment that may linger on for a few months or more.
Serious rectal/bladder injury is fortunately an uncommon
event. It is extremely rare to require surgery or long-term
medical management to treat chronic radiation effects to
normal tissues. It is expected that the lower dose of
radiation that the bladder and rectum receive as a consequence of the use
of 3DCRT will result in even fewer
long-term deleterious effects.
Is 3D conformal radiation therapy better than conventional
radiation therapy?
3DCRT is a relatively new
technology and until recently has been available at only a
few academic institutions [5]. Data on long-term
effectiveness are sparse, but early data have convincingly demonstrated that
the volume of normal bladder and rectum receiving a high dose
of radiation therapy is substantially reduced. Some
institutions have demonstrated that early acute side effects
are reduced with the use of 3DCRT [6].
Others have demonstrated that equal side effects are seen in
patients treated with 3DCRT compared to conventional radiotherapy despite
being treated with higher radiation doses using 3DCRT [7].
A recent report from by the Fox Chase Cancer Center in
Pennsylvania has demonstrated an improved outcome as
measured by disease-free survival based on PSA data (PSA < 1.5 ng/ml
and not rising after
treatment). These encouraging results were reported with 3DCRT
using standard, non-escalated radiation therapy
doses [8].
What studies are currently ongoing investigating 3DCRT for prostate cancer?
One of the theoretical advantages of 3DCRT is that the
smaller volumes of normal
tissue receiving a high dose will allow more safe escalation
of radiation therapy dose to the prostate cancer. Mature
studies have demonstrated that the likelihood of controlling
prostate cancer with radiation therapy is dependent on the
amount of radiation delivered [3, 4]. Higher
doses appear more effective at controlling more cancers.
Prior to the availability of 3DCRT, radiation
oncologists were restricted to moderately high doses because
of the risks of bladder and rectal toxicity. The radiation
oncologist could not give the prostate an extremely high dose
because he/she was limited by what the bladder and rectum
would tolerate. Now, with the use of 3DCRT,
several institutions are conducting trials of
escalated doses of radiation therapy for prostate and other
cancers. Once the safest high dose of radiation therapy is
determined, it is expected that a randomized study will be
conducted comparing high dose 3DCRT to
standard dose radiation therapy to determine whether or not
the higher dose of radiation therapy is truly more effective.
Currently, a nationwide dose escalation study is being
conducted jointly by the 3D Oncology Group and the Radiation
Therapy Oncology Group. An initial cohort of patients were
treated at doses of 68.4 Gy and patient accrual is currently
ongoing at a dose of 73.8 Gy. If no serious side effects are
encountered at this level (and none have been to date), then
patients will be treated at doses of 79.2 Gy. Some institutions have
already used 3DCRT to treat patients with doses as high as 81
Gy with no increase in severe late complication rates [9].
Administering this level of radiation dose would not have
been safe without the use of 3DCRT
planning.
What will the future hold for 3DCRT and the treatment of prostate cancer?
Even as patients are currently being treated with 3DCRT,
technological developments are
further improving the ways in which radiation therapy will
be delivered in the future.
Research is being conducted to
minimize the effects of internal organ motion on treatment
delivery. If prostate movement and daily setup variations
can be minimized, then even more tightly shaped conformal
dose distributions will be possible.
Some technology, such
as proton beam therapy, may benefit from improved target
localization. Eventually, the use of radiation beam
intensity modifiers, such as a dynamic multi-leaf collimator,
will be used while the radiation beam is delivering dose and
"sculpt" conformal radiation therapy dose distributions
tightly to levels similar to that seen with proton beam
therapy. This process of beam intensity modulation is
currently being used by some radiation therapy clinics in
tumor sites other than the prostate. It will not be too long
before it is used in high dose radiation therapy for prostate
cancer.
References
1. Ten Haken RK, Perez-Tamayo C, Tesser RJ, et al: Boost
treatment of the prostate using shaped fixed fields. Int J
Radiat Oncol Biol Phys 1989; 6: 193.
2. Sandler HM, McShan DL, Lichter AS: Potential
improvement in the results of irradiation for prostate
carcinoma using improved dose distribution. Int J Radiat
Oncol Biol Phys 1991; 22: 361.
3. Hanks GE, Martz KL, Diamond JJ: The effect of dose on
local control of prostate cancer. Int J Radiat Oncol Biol
Phys 1988; 15: 1299.
4. Perez CA, Pilepich MV, Zivnuska F: Tumor control in
definitive irradiation of localized carcinoma of the
prostate. Int J Radiat Oncol Biol Phys 1986; 12: 523.
5. Meyer JL, Purdy JA (eds): 3-D Conformal Radiotherapy
(Frontiers in Radiation Therapy and Oncolology, vol 29) Basel, Karger, 1996.
6. Soffen EM, Hanks G, Hunt MA, et al.: Conformal static
field radiation therapy treatment of early prostate cancer
versus non-conformal techniques: A reduction in acute
morbidity. Int J Radiat Oncol Biol Phys 1992; 24: 485.
7. Pollack A, Zagars GK, Starkschall G, et al: Conventional
vs. conformal radiotherapy for prostate cancer:
Preliminary results of dosimetry and acute toxicity. Int J
Radiat Oncol Biol Phys 1996; 34: 555.
8. Hanks G, Lee WR, Schultheiss TE: Clinical and
biochemical evidence of control of prostate cancer at 5
years after external beam radiation. J Urol 1995; 154: 456.
9. Zelfefsky MJ, Leibel SA, Kutcher GJ, et al: The
feasibility of dose escalation with three-dimensional
conformal radiotherapy in patients with prostatic
carcinoma. Cancer J Sci Am 1995; 1: 142.
Editorial comment
This article offers a useful introduction to three-dimensional conformal radiation therapy
for the interested patient. As the authors note, it is not a
detailed scientific review. 3DCRT is a form of therapy that is in a stage
of rapid evolution as more radiation oncologists and radiation therapists
are exposed to this technique. It is certain that the ability to
maximize quality of outcome depends upon the experience and expertise
of the radiotherapy team. Thus, patients may wish to consider this
experience and expertise in deciding whether to seek 3DCRT at specific
medical centers.
In the long term, The Prostate Cancer InfoLink expects 3DCRT to lead to
lower levels of adverse reaction with better survival than has been the
case in the past for prostate cancer patients undergoing radiation therapy.
However, the ability of radiation therapy to cure prostate cancer is
still dependent upon the ability to actually kill all of the
viable prostate cancer cells. Whether 3DCRT is actually able to significantly
improve on this ability compared to conventional, standard radiotherapy
is still an unanswered question.
[This editorial comment was part of the original page.]
|
|